Most people with depression feel better with treatment. But about 30 percent can’t seem to shake off their depression. This is especially true if you respond poorly — or don’t respond at all — to antidepressants.
For those with treatment-resistant depression, a noninvasive treatment called transcranial magnetic stimulation (TMS) offers hope.
This relatively new option can bring relief when other treatments for depression fail, says psychiatrist Murat Altinay, MD.
How TMS works
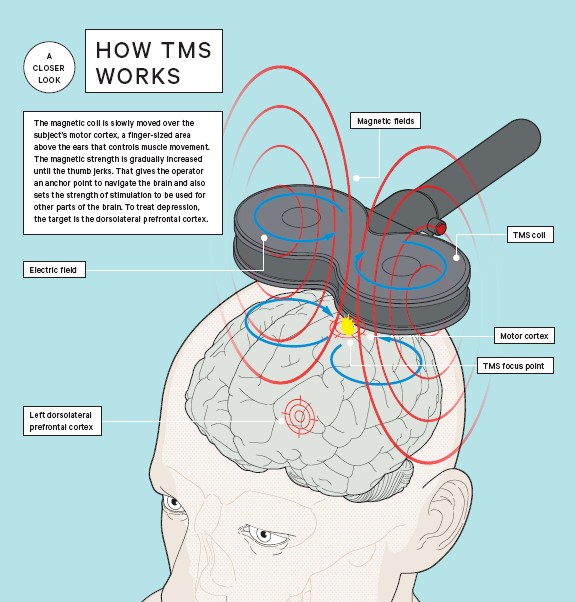
TMS uses a magnetic field — similar to that used in magnetic resonance imaging (MRI) — to stimulate the brain’s dorsolateral prefrontal cortex, which plays a key role in mood.
Increasing the activity of neurons in this area lessens depression, Dr. Altinay explains. Having your brain stimulated by a magnetic field may sound a bit scary, but the experience isn’t painful.
“The typical TMS session lasts about 30 to 40 minutes,” he says. “During the session, patients are fully awake and sitting in a comfortable chair.”
Here’s what happens:
- The doctor places the TMS coil on the top left side of your head.
- The coil delivers stimulation for about 4 seconds, stops for about 15 seconds, then starts again.
- This cycle repeats about 75 times per session.
- During stimulation, you hear a tapping sound and feel a tapping on your scalp. “Those who are a little more sensitive may experience some scalp discomfort,” Dr. Altinay says.
Throughout treatment, you are fully aware of what’s going on. You can speak, read or even nap. After treatment, you can resume your daily activities immediately without restrictions, he says.
One drawback of TMS is that it’s time-consuming, at least in the beginning. During the first phase, you’ll likely receive treatment every weekday for six weeks (about 30 times).
During the second (maintenance) phase, the doctor tailors the frequency to meet your needs. You may get treatments every other week, monthly, or every two months. The frequency gradually decreases.
TMS: Effective and safe
Research shows that regular maintenance with TMS helps prevent recurrence and reduces the symptoms if depression should come back.
TMS has relatively few side effects. “The most frequent side effect is headache, but not everybody experiences that,” Dr. Altinay says. If you do get headaches, taking Advil® or Tylenol® before treatments can help.
More serious is the increased risk of seizures reported in the literature. “Having a seizure disorder would prevent a patient from being the best candidate for TMS. However, I’ve been doing TMS for 10 years, and none of my patients have experienced seizures,” he notes. “Some literature suggests that if a seizure disorder is well-controlled with anti-epileptic drugs, TMS might still be an option.”
Who can benefit from TMS
Dr. Altinay says TMS mainly targets those who don’t respond adequately to antidepressants or who are completely medication-resistant. TMS also can be offered if antidepressants cause severe reactions or side effects, or worsen other health issues. However, TMS is not recommended for anyone with a:
- Poorly controlled seizure disorder
- Metallic implant close to the head
- Brain tumor or brain disease
- Substance abuse disorder
How TMS differs from ECT
You may have heard of another treatment for medication-resistant depression: electroconvulsive therapy (ECT), inaccurately called “shock therapy.”
While TMS and ECT share similarities, TMS offers several advantages:
- Both techniques rely on stimulation, but ECT uses electrical energy to stimulate the entire brain. “You can’t control which area you stimulate with ECT,” says Dr. Altinay. The global brain stimulation, coupled with the need for anesthesia, often causes short-term memory loss.
- TMS uses a magnetic field instead of electrical energy and stimulates only the part of the brain involved in depression. This results in fewer side effects. “In fact, TMS has actually been shown to enhance memory,” he adds.
Only a limited number of healthcare providers offer TMS, so it may take some research to find one near you. And not all health insurance companies will pay for TMS, says Dr. Altinay.
However, this option offers hope for those who’ve struggled to find relief from depression through traditional avenues, he says.